Center for Global Health: Creating a Healthier World
 Pitt’s Sharon L. Hillier (third from left in yellow shirt) meets with local women and (on Hillier’s left) their tribal chief in Blantyre, Malawi, where the Microbicide Trials Network (MTN) operates a site. Hillier is an internationally recognized microbiologist who is the principal investigator for the MTN, an HIV/AIDS clinical trials network established by the National Institute of Allergy and Infectious Diseases. She is also a professor and vice chair for faculty affairs and director of reproductive infectious disease research in the Department of Obstetrics, Gynecology, and Reproductive Sciences in Pitt’s School of Medicine. In her role at MTN, Hillier leads an international team of investigators and community and industry partners from seven countries and three continents, directing an ambitious HIV-prevention research agenda.
Pitt’s Sharon L. Hillier (third from left in yellow shirt) meets with local women and (on Hillier’s left) their tribal chief in Blantyre, Malawi, where the Microbicide Trials Network (MTN) operates a site. Hillier is an internationally recognized microbiologist who is the principal investigator for the MTN, an HIV/AIDS clinical trials network established by the National Institute of Allergy and Infectious Diseases. She is also a professor and vice chair for faculty affairs and director of reproductive infectious disease research in the Department of Obstetrics, Gynecology, and Reproductive Sciences in Pitt’s School of Medicine. In her role at MTN, Hillier leads an international team of investigators and community and industry partners from seven countries and three continents, directing an ambitious HIV-prevention research agenda.The human immunodeficiency virus (HIV) is so adept at eluding the immune system that by the time the body recognizes one version of the virus, that version may already have mutated three or four times.
Mycobacterium tuberculosis, the rod-shaped bacterium that causes tuberculosis (TB), is carried by two billion people on the planet. It hides out in tiny, oxygen-deprived pockets deep inside the carrier’s lungs and can be transmitted by a sneeze.
The H1N1 virus is the latest in a series of influenzas that have mutated in pigs, birds, and people. Its 1918 predecessor killed more than 50 million people worldwide.
These diseases affect billions of people. They can thwart economic development, roil political systems, and dislodge whole societies. And in today’s increasingly global and mobile society, they can spread within hours.
To combat these and other diseases, a growing scientific field has emerged: global health. Once thought of as a cottage industry within medicine—the domain of a few daring medical missionaries and biomedical explorers—today the field is attracting the interests of epidemiologists, virologists, biostatisticians, and computer modelers.
“We’re much more interconnected, and the health challenges we face in this country can’t be separated anymore from the rest of the world,” says Helene Gayle, president and CEO of CARE, the global humanitarian nonprofit organization. “It’s not so much that we’re doing something to take care of ‘these’ people and exotic diseases in faraway countries. We all have something to learn, and it’s in our own interest to focus on a more global way of looking at disease.”
Pitt’s Center for Global Health
The University of Pittsburgh, a national powerhouse in the health sciences, added its considerable weight to these efforts with the creation of the Center for Global Health. Developed with a grant from the University, the center was established to coordinate, support, and expand global health research at Pitt by bringing under one umbrella the institution’s many renowned scientists and medical researchers working in the global health arena.
This University-wide multidisciplinary center combines existing strengths in health and biomedical research with those in other disciplines by partnering with schools across the University. “Most global health problems are rooted in a combination of health, education, social, economic, political, and environmental factors and call for integrated, multidisciplinary approaches,” says Joanne Russell, director of the center. “We want the center to be a portal for academics across the University as well as a bridge between disciplines.”
In the health sciences, the Pitt schools that collaborate with the center include medicine, public health, nursing, pharmacy, dentistry, and health and rehabilitation sciences. In addition, there are existing collaborations with the School of Law, the Graduate School of Public and International Affairs, and the School of Arts and Sciences, as well as with the University Center for International Studies.
“The center is a catalyst for change,” says Donald S. Burke, associate vice chancellor for global health and UPMC-Jonas Salk Professor of Global Health. Burke, who also is dean of Pitt’s Graduate School of Public Health and a veteran epidemiologist in the field of infectious disease, is the driving force behind the center. “The center is designed to foster action. We are not trying to be the problem solvers ourselves, but we help academic researchers get what they need to pursue some of these important health questions in international settings.”
HIV, TB, genetics, and maternal and child health are just some of the areas studied by Pitt’s global-health researchers. The center helps Pitt—the No. 5-ranked biomedical research university in the country, as measured by total National Institutes of Health (NIH) grants received—to export its considerable bank of expertise by training researchers worldwide.
The center links graduate students with mentors and host sites around the world through which they pursue global health projects. This includes working in health clinics or providing primary care in the developing world. But Burke stresses that the ultimate focus of the center is research.
“A lot of the time when people think of global health, it’s from a missionary and humanitarian perspective,” Burke says. “It’s noble, it’s important, and it’s useful, but I think that we, as an academic institution, have as our job the definition and solution of problems, and to do that we need a research focus.”
Burke began his career as a medical officer with the U.S. Army, retiring with the rank of colonel. While researching infectious diseases with the Army, Burke helped conduct pioneering trials in Thailand for Japanese encephalitis vaccine. The trials proved the effectiveness of a drug that now protects 30,000 to 40,000 children from paralysis or death each year.
In 2006, Burke came from Johns Hopkins University to Pitt because “what I saw was a university that had an extraordinary potential to make a difference in people’s lives around the world,” he says. “I thought, ‘Here you’ve got this combination of outstanding people and growing expertise that could be brought to bear on some of the world’s biggest problems. This is a great place to help make important things happen.’ ”
Global Partnerships: Breaking an Antiquated Cycle
Many of the developing world’s biggest problems are exacerbated by severe medical crises. High rates of HIV, TB, and malaria in sub-Saharan Africa, for example, contribute to the region’s toxic brew of poverty, political instability, and dislocation. These problems, in turn, worsen many countries’ ability to fight public health problems. Half of the deaths in the developing world are caused by infectious diseases, almost all of them either treatable or preventable.
“It’s a vicious cycle,” says David Heymann, a longtime World Health Organization (WHO) official and current chair of the British Health Protection Agency, the United Kingdom’s equivalent of the Centers for Disease Control and Prevention (CDC). “Only healthy people can help their countries move out of poverty, and when these countries move out of poverty, they contribute to global production and the world market.”
To climb out of poverty, developing nations must build the human capital necessary to monitor, treat, and prevent public health problems. This is an area where academics, like those in Pitt’s Center for Global Health, can have an impact. An example of building this kind of capacity can be seen in a Pitt-led project in Brazil. Lee Harrison, a professor of medicine, epidemiology, and infectious diseases and microbiology, has helped train scores of Brazilian HIV researchers over the past two decades. Many of these researchers now receive CDC and NIH grants to conduct their work.
For Harrison, a senior investigator affiliated with the Center for Global Health, the project highlights the public health field’s progress. Decades ago, “parachute research” was the norm in the developing world: “Somebody from the United States or Europe parachutes in, does his or her research project, and leaves, and the country’s no better off than it was when he or she got there. That has totally changed.”
A partnership with a host institution, Harrison says, is a way to leave a lasting effect on the public health infrastructure of a country. One by one, the parachutes are being mothballed. Today, the Brazilian researchers trained through Pitt are testing new HIV vaccines and conducting studies to improve the delivery of anti-HIV medications in the developing world.
“Brazil has become a world-class training site,” Harrison says. “We provided this training and started to develop a research infrastructure. That, in turn, led to data that we were able to show funding agencies looking for sites to do trials on microbicides and for HIV vaccines.
“The idea is to create the infrastructure that will allow you to compete for funding and become a site to do these kinds of studies,” Harrison adds. “In Brazil, we’ve seen the fruits of the infrastructure we helped build. We’re planting the seeds now in Mozambique.”
Education and Training: Building the Infrastructure
 Pitt researchers Deborah McMahon and Lee Harrison visit a laboratory supervisor and technicians in the Catholic University of Mozambique’s (UCM) Infectious Diseases Research Center in Beira, Mozambique. McMahon (front row, center), a Pitt professor of medicine and of infectious diseases and microbiology, is the project director for Beira’s Twinning Center, an HIV-focused health center where Pitt and UCM faculty train local health care workers in primary HIV care. Harrison, (back row, far right), a Pitt professor of medicine, epidemiology, and infectious diseases and microbiology, has helped train scores of Brazilian HIV researchers over the past 12 years. He and McMahon are discussing how U.S. and Brazilian researchers could train their Mozambique counterparts through an HIV research training program funded by the National Institutes of Health Fogarty International Center.
Pitt researchers Deborah McMahon and Lee Harrison visit a laboratory supervisor and technicians in the Catholic University of Mozambique’s (UCM) Infectious Diseases Research Center in Beira, Mozambique. McMahon (front row, center), a Pitt professor of medicine and of infectious diseases and microbiology, is the project director for Beira’s Twinning Center, an HIV-focused health center where Pitt and UCM faculty train local health care workers in primary HIV care. Harrison, (back row, far right), a Pitt professor of medicine, epidemiology, and infectious diseases and microbiology, has helped train scores of Brazilian HIV researchers over the past 12 years. He and McMahon are discussing how U.S. and Brazilian researchers could train their Mozambique counterparts through an HIV research training program funded by the National Institutes of Health Fogarty International Center.In Beira, Mozambique, Pitt initially established a partnership with the Universidade Católica de Moçambique (UCM). In June 2009, the two institutions opened the Twinning Center, an HIV-focused health center to train local health care workers in primary HIV care. Funded by the U.S. President’s Emergency Program for AIDS Relief, the center includes faculty from the Pitt School of Medicine’s HIV/AIDS Program and UCM’s Faculty of Medicine.
Mozambique is one of the 10 poorest countries in the world, with an HIV-infection rate that exceeds 16 percent nationally and 26 percent in the Beira region. The country has a patient-to-doctor ratio of 33,500 to one; in the United States the rate is 390 to one.
“In the rural areas, the chances of ever seeing a doctor are low,” says Deborah McMahon, project director for the Twinning Center and a Pitt associate professor of medicine and of infectious diseases and microbiology. “We are trying to develop health care capacity in Mozambique that will improve access to HIV care.”
The newly renovated St. Luke’s Health Center in Beira already has provided primary care to more than 1,300 local residents since opening in June 2009. “In the beginning, the center saw only a few dozen patients a day,” says McMahon. “Now there are between 75 and 100 patients a day. It is getting increasingly busier as the community learns about the center.”
At St. Luke’s, nurses, physician’s assistants, medical students, and other health care workers receive hands-on mentored training, the backbone of Western-style medical education. It eventually will become a one-stop location for HIV patients.
“Medical staff see patients with diarrheal illnesses, parasitic infections, fever, pneumonia, HIV, TB, malaria, and chronic conditions like diabetes and high blood pressure,” McMahon says. At least one Pitt faculty member is at the center every day to supervise training and care. “This hands-on training helps these health care workers on the front lines of primary care in Mozambique, where care is needed the most.”
Countries like Mozambique have a tremendous need not only for trained caregivers, but also for homegrown researchers who can identify and solve problems. Each country or region faces different problems—strains of HIV vary from country to country, for instance, and drugs developed in the United States may not work the same way in Mozambique. Exporting a therapy developed in one country to another may require adaptation.
Seeing an opportunity to take advantage of some intriguing synergies between Brazil and Mozambique, Harrison and other Pitt faculty members explored opportunities to begin a research training program in Beira. Pitt’s Twinning Center in Beira offered a ready-made host site. In addition, both Brazil and Mozambique share a common language: Portuguese. Harrison is now planning “south-to-south” trainings that will allow Brazilian researchers to train their counterparts in Mozambique.
The program is funded with a $2.8 million grant from NIH’s John E. Fogarty International Center for Advanced Study in the Health Sciences, which focuses on improving medical research in the developing world. With the grant, Pitt is developing a research training site in Mozambique and expanding programs already under way in Brazil and India.
Providing New Tools: Research Collaboration
 Vishwajit L. Nimgaonkar (second from right), a Pitt professor of psychiatry and human genetics, has been training researchers in India and Egypt in the genetic studies of psychiatric disorders. Nimgaonkar is pictured here in Mansoura, Egypt, with two other Pitt professors: Rohan Ganguli (center), a professor of psychiatry, pathology, and health and community systems in Pitt’s School of Medicine, and Konasale M. Prasad (far right), an assistant professor of psychiatry. They were visiting two Egyptian psychiatrists (pictured on left) who are collaborating with Nimgaonkar on his research.
Vishwajit L. Nimgaonkar (second from right), a Pitt professor of psychiatry and human genetics, has been training researchers in India and Egypt in the genetic studies of psychiatric disorders. Nimgaonkar is pictured here in Mansoura, Egypt, with two other Pitt professors: Rohan Ganguli (center), a professor of psychiatry, pathology, and health and community systems in Pitt’s School of Medicine, and Konasale M. Prasad (far right), an assistant professor of psychiatry. They were visiting two Egyptian psychiatrists (pictured on left) who are collaborating with Nimgaonkar on his research.While Harrison and others train physicians around the world in infectious disease research, another Pitt researcher and Center for Global Health scholar is training doctors to study another epidemic that is more difficult to detect. For the past 20 years, Vishwajit Nimgaonkar, professor of psychiatry and human genetics, has been training researchers in India and Egypt in the genetics of psychiatric disorders.
Nimgaonkar says the research is badly needed: WHO reports that mental health disorders, like schizophrenia and bipolar disorder, are the third-leading cause of disability worldwide. About 1 percent of the world’s adult population suffer from schizophrenia. Advances in computational biology and gene mapping now allow researchers like Nimgaonkar to plumb millions of DNA base pairs to look for genetic markers for mental health disorders.
These methods work best with a broad spectrum of genetic samples, so the team is collaborating with psychiatric researchers around the world to increase the pool of DNA being studied. In the process, team members are looking at whether environmental factors—nutrition, exposure to disease, and traumatic episodes—play a role in the development of psychiatric disorders.
Nimgaonkar-trained psychiatrists at India’s University of Delhi are now conducting research of their own; one initiated an intriguing study of the effects of yoga on people with schizophrenia. “These researchers bring insights that we may not necessarily have, because they have different experiences and backgrounds,” Nimgaonkar says. “Clinicians in these countries are likely to have more experience than we do because they see many more patients than we do. What they’re lacking are the tools to do research, and they want to be researchers. They realize there is a benefit to doing research.”
Informing Policy: Modeling Infectious Disease Patterns
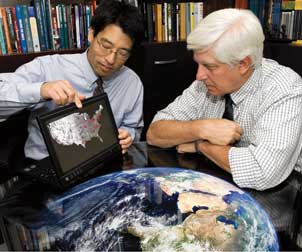 Pitt researchers are helping control the spread of infectious diseases virtually, thanks to a $13.4 million National Institutes of Health grant that established the Models of Infectious Diseases Agent Study (MIDAS) National Center of Excellence at the University of Pittsburgh. Headed by Donald S. Burke, dean of Pitt’s Graduate School of Public Health (GSPH) and associate vice chancellor for global health, the center is developing, testing, and employing computer simulations to help public health officials and other decision makers predict infectious disease outbreaks and intervene to control them. Pictured are Burke (right) and Bruce Y. Lee, an assistant professor in GSPH and a core member of the recently founded Public Health Dynamics Laboratory, analyzing a map showing the spread of influenza throughout the United States.
Pitt researchers are helping control the spread of infectious diseases virtually, thanks to a $13.4 million National Institutes of Health grant that established the Models of Infectious Diseases Agent Study (MIDAS) National Center of Excellence at the University of Pittsburgh. Headed by Donald S. Burke, dean of Pitt’s Graduate School of Public Health (GSPH) and associate vice chancellor for global health, the center is developing, testing, and employing computer simulations to help public health officials and other decision makers predict infectious disease outbreaks and intervene to control them. Pictured are Burke (right) and Bruce Y. Lee, an assistant professor in GSPH and a core member of the recently founded Public Health Dynamics Laboratory, analyzing a map showing the spread of influenza throughout the United States.In addition to providing education and training in many locations worldwide, the Center for Global Health is making an impact at the highest levels of public health policy through its research.
The Vaccine Modeling Initiative, a group of researchers based at Pitt, was at the forefront of helping to steer the U.S. government’s response to the H1N1 virus as well as to other infectious diseases around the world. The project has commanded the attention of the world health community, and it has received a $10 million grant from the Bill and Melinda Gates Foundation, which funds projects dedicated to the eradication of infectious disease.
The initiative is headed by Burke, who began using computer modeling in the 1990s to predict the behavior of diseases. “Computer models allow us to test our theories in silica,” Burke says. “For a number of reasons, you can’t test these hypotheses in a live population.”
Computers are useful, Burke says, because diseases behave according to a set of numbers—transmission rates, latency periods, and the length of time a carrier remains contagious. As computing power has increased, modelers have been able to simulate how a broad range of variables might impact the outcome of a disease. Population density, the distance people travel to work, and the speed at which a virus spreads can all be plugged into an algorithm.
WHO, the CDC, and the U.S. Department of Homeland Security used Burke’s simulations in 2004 to plan for a possible avian influenza outbreak. That same year, WHO arranged to keep three million vaccine doses on hand in Southeast Asia based on the model’s calculation of the number of doses that would be needed to thwart an outbreak. “We basically built an artificial society of millions of persons based on census, transportation, and other demographic and sociological data,” Burke says.
In 2009, the U.S. Department of Health and Human Services asked Pitt’s modeling group to derive a model for the H1N1 virus, or “swine flu.” Over the summer, the group began inputting new data on how the virus behaved in the Southern Hemisphere’s flu season in Australia, New Zealand, and South America. At the time, Burke said that initial reports showed an excess of mortality rates in young adults, which “will help us determine where we should be putting our resources.” The models do not tell policymakers what to do, Burke notes. Rather, they provide detailed information on the likely ramifications of the decisions they make.
The group also uses modeling to help simulate vaccine delivery in West Africa for a variety of diseases, including dengue fever and measles. “By modeling the vaccine supply chains of entire countries, we can help decision makers test how different strategies and changes may affect vaccine delivery and disease control,” says Bruce Lee, Pitt assistant professor of medicine, epidemiology, and biomedical informatics. Working with WHO and host-country health officials, the group incorporates all the variables necessary to get a vaccine to a clinic—right down to the number of doses in each package and the size of refrigerated storage space.
The Central Agenda: Pushing the Boundaries in Research
As Burke noted earlier, for an academic institution like Pitt to have a long-term impact, it must focus on the problem-solving aspects of worldwide health issues—with a central agenda on global research. From HIV to TB to the genetics of birth defects, the University’s robust research engine is helping to discover novel therapies, interventions, and diagnostic tools using a broad array of techniques.
More and more, researchers are working in a global context, says Sharon Hillier, Pitt professor of obstetrics, gynecology, and reproductive sciences and of microbiology and molecular genetics. Hillier is head of the Microbicide Trials Network, which is piloting a study of 5,000 women in five countries in sub-Saharan Africa to test the efficacy of topical microbicides and prophylactic use of antiretroviral drugs (ARVs) to prevent sexual transmission of HIV.
“The old idea was that when you worked in global health, you were really trying to develop and deliver medicines to populations that didn’t have enough doctors or enough medicine. Many people thought it wasn’t possible to do good clinical research in those settings because there wasn’t sufficient research infrastructure,” says Hillier. “What we’ve learned is that you can do outstanding clinical research with these populations in the developing world as well as for women living in wealthy countries like the United States. Many people are surprised to hear that the trials done in the developing world will help find ways to reduce the spread of HIV in American women, too.”
No Miracle Cure for HIV: The Microbicide Trials Network
 Phalguni Gupta is the principal investigator of a $7.2 million grant from the National Institute of Allergy and Infectious Diseases to develop microbicides against HIV transmission. Gupta is a professor and assistant chair in the Pitt Graduate School of Public Health’s Department of Infectious Diseases and Microbiology.
Phalguni Gupta is the principal investigator of a $7.2 million grant from the National Institute of Allergy and Infectious Diseases to develop microbicides against HIV transmission. Gupta is a professor and assistant chair in the Pitt Graduate School of Public Health’s Department of Infectious Diseases and Microbiology.Hillier’s research comes at a time when perspectives on the HIV pandemic are shifting. An AIDS vaccine, once thought to be on the near horizon, is now considered to be many years away. And while ARVs have helped millions infected with HIV to live longer, they are not available to everyone who needs them. The pandemic continues to grow—33 million people worldwide, two-thirds of them in sub-Saharan Africa, are HIV positive—even as the public’s fear of the disease has ebbed.
“People like to embrace the notion that HIV transmission has leveled off and AIDS is more manageable,” says Hillier. “The problem is that when people become infected, they are infected for life, and there’s a huge health cost and personal burden for people who carry HIV. For every two people who begin treatment, four or five people are newly infected. Without new methods of prevention, we cannot gain ground against the epidemic.”
For proof of the epidemic’s staying power, Hillier points to South Africa, where several Microbicide Trials Network sites are located. In the city of Durban, of the young women screened for the trials, between 35 and 40 percent test positive for HIV. “When you meet people in South Africa, it’s very hard to find someone who doesn’t have a cousin, a brother, an aunt, or an uncle who’s been affected by AIDS,” she says.
Hillier’s is the first study of its kind to examine both a microbicide and an oral ARV pill in high-risk women. These prevention methods, if proven effective, could be particularly powerful in sub-Saharan Africa, where women make up 60 percent of the adult HIV population and, in many instances, have difficulty negotiating condom use with their partners.
“We’ve spent a lot of time thinking of ways to give women drugs to stop transmission from the HIV-infected mother to her baby. But how much better it would be to prevent moms from getting infected in the first place.” Hillier says. “That’s a much more powerful goal, I think.”
How New Viruses Emerge: The Virus Hunter
Viruses are among the most abundant and successful species on earth. They also are responsible for much of human suffering: HIV, influenza, encephalitis, and a host of other deadly diseases are by-products of viral success. What makes viruses especially dangerous is their ability to mutate and jump from one species to the next. SARS, avian influenza, H1N1, and HIV have all entered the human population from other animal carriers. One Pitt researcher is traveling around the world to find out how new viruses are created and what specific mechanisms they use to jump carriers.
James Pipas, professor of biological sciences, is traveling to swamps and meadows looking for clues to virus mutation. He is testing a hypothesis that viruses can interchange large swaths of their DNA. Called recombination, these gene swaps could explain how viruses mutate and jump species. A virus carried by a zebra, for instance, could conceivably swap DNA with a rhinoceros-borne bug and equip itself to jump carriers. Pipas developed an algorithm based on factors like biodiversity and the prevalence of rare species to predict the most likely hot spots for gene recombination.
The first place the model told him to look was southern Siberia, an area covered with shallow marshes and endless expanses of tick-filled grassland. As ticks are notorious virus hosts, Pipas is now trying to organize the largest tick collection in the world. “We think this type of genetic exchange could be contributing to emerging infectious diseases,” says Pipas. “We want to go to nature and look for this process.”
Pipas also has begun research on viruses in Borneo, Malawi, and Tibet. What he finds there could yield clues as to how new viruses emerge and why the diseases they cause continue to confound us.
Genetics: Tracking the Origins of a Birth Defect
Cleft palate and cleft lip are among the most common birth defects in the world, and in developing countries they can be deadly if not treated properly. Clearly, these are genetically based defects, but scientists are still uncertain about the exact mechanisms by which parents pass them along to their children. The defects occur in about one in 700 births.
“That’s a huge number,” says Mary Marazita, professor of oral biology, human genetics, and psychiatry. “In contrast, most birth defects affect about one in 5,000 or even one in 100,000 births.”
Marazita studies the genetics of these birth defects to understand better their underlying causes. Her goal is to provide improved genetic counseling to parents and superior diagnostic tools for surgeons to improve outcomes for cleft patients.
“Facial defects are really hard on families,” explains Marazita, “There’s a lot of stigma around facial differences because humans are very attuned to faces. Anything to do with the face can have a big impact on your relationship with other people.”
The impact of these birth defects is particularly daunting in the developing world, where one in three newborns with a cleft palate doesn’t survive because it is extremely difficult for them to ingest food.
A series of surgeries can greatly reduce both the defect and the number of years of dental procedures and speech therapy. The average cost of caring for a child born with a cleft lip and palate in the United States is between $100,000 and $200,000.
Marazita’s group has found other more subtle facial defects that could signify whether a parent has a greater risk of passing on cleft lip or palate to his or her child. She collaborates with researchers around the world, from big-city surgical wards in China to rural clinics in Patagonia, to compile as much genetic detail on clefts as possible. Assembling a wide variety of study participants from Europe, Asia, and the Americas is helping Marazita and her collaborators track down the genetic clues to clefts.
“To gain a full understanding of the genetic and environmental factors that lead to clefts depends on getting to other parts of the globe,” Marazita says, “and it’s really bearing fruit for our research.”
Probing the Depths of TB
 Joanne Russell is director of Pitt’s Center for Global Health. Once the domain of individual medical missionaries and biomedical explorers, global health has evolved into a scientific field that includes specialties ranging from epidemiology and virology to biostatistics and computer modeling. Pitt’s center aims to tackle health challenges in a world that is becoming increasingly interconnected.
Joanne Russell is director of Pitt’s Center for Global Health. Once the domain of individual medical missionaries and biomedical explorers, global health has evolved into a scientific field that includes specialties ranging from epidemiology and virology to biostatistics and computer modeling. Pitt’s center aims to tackle health challenges in a world that is becoming increasingly interconnected.Among the world’s most dangerous diseases, tuberculosis (TB) has been with us for a long, long time: The bones of Egyptian mummies showed signs of tubercular decay. In the 1940s, U.S. researchers discovered powerful antibiotics that controlled the disease in the Western world, but the emergence of HIV has made TB an ever-more deadly disease in less-developed countries. When HIV suppresses the immune system, an otherwise resistant TB carrier succumbs more easily. This double epidemic of HIV and TB is prevalent in the developing world, where 1.6 million people die annually from TB.
So, understanding TB’s molecular pathways is crucial in developing ways to slow this resilient disease. Among those at the forefront of the field is JoAnne Flynn, Pitt professor of microbiology and molecular genetics, medicine, and immunology.
Flynn says that the reason TB is such a resilient killer is that the bacterium that causes it, Mycobacterium tuberculosis, is uniquely designed to hide inside the body. “It’s evolved incredibly with humans,” says Flynn. “It’s been in people since we became people. What you have is a really successful pathogen. It has a lot of ways to survive.”
One way TB survives is by lying in wait: It lies dormant in about 95 percent of its carriers. Flynn and her collaborators discovered that the bacterium can survive within a cluster of immune cells—called a granuloma— inside the human lung. Conditions in some parts of some granulomas are anaerobic—meaning there is no oxygen, a state that would kill most invaders. But some TB strains can survive in that state for years, until the host’s immune system is compromised enough for the bacterium to replicate.
Flynn and her collaborators have developed a novel way of tracking the granulomas inside the lung by using advanced imaging to monitor in real time how TB tracks a carrier. She can study where granulomas form and how the immune system rushes to respond to a new bacterium. “There’s nobody else doing this,” Flynn says. “It’s going to make a difference in how we deal with tuberculosis.”
Flynn says that the Center for Global Health will help lab researchers like her by allowing for closer interaction with other researchers who deal with TB in the developing world, where rates are much higher than they are in the United States: “We can ask them, ‘What are you really seeing on the ground?’ We can get access to places where there are a lot more people with TB. It will also help us with our ultimate goal of putting on clinical trials in the field.” Ultimately, Flynn thinks, this research could lead to a cure.
Paving the Way to the Future
Many, many more Pitt faculty than have been mentioned here are working in various facets of global health, from researching the root cause of illness, to training others to fight disease, to helping to guide policymakers in product development, public preparedness, and other policy matters. The University’s researchers are committed to fighting disease, improving the quality of life, and creating a healthier world.
Thanks in part to the efforts of scientists at Pitt, global health is increasingly becoming centered on long-term collaborations and partnerships between institutions with similar missions and goals. A new project supported by the Center for Global Health involves collaborative research with Wuhan University in Wuhan, China, Pittsburgh’s sister city. Pitt faculty members are sharing their expertise as Wuhan works to address environmental issues, particularly air pollution. The goal of the project is to examine the relationship between various pollutants and hospitalizations for specific cardiovascular and respiratory diseases in Wuhan. The Center also supports a collaboration with the University of Pittsburgh Medical Center (UPMC) International in Palermo, Italy, in which researchers are investigating ways to prevent liver transplant recipients from being re-infected with the Hepatitis C virus. Future partnerships also are expected to include joint programs with UPMC International in Ireland, and the United Kingdom, and Qatar. In addition, the Center for Global Health expects to play a major role in creating leaders for a global society and was approved as a host institution (along with Pitt’s Graduate School of Public Health) for the Hubert H. Humphrey Fellowship Program beginning last semester.
If all of this sounds like a big challenge, Burke says, that’s because it is: “We need to bring every tool at our disposal to this job, because the job is too important, and these problems are too serious for us to take them lightly. We are entering a period where we are all learning to work together on these problems because we have to. That is the vision for this Center for Global Health.”
Other Stories From This Issue
On the Freedom Road

Follow a group of Pitt students on the Returning to the Roots of Civil Rights bus tour, a nine-day, 2,300-mile journey crisscrossing five states.
Day 1: The Awakening
Day 2: Deep Impressions
Day 3: Music, Montgomery, and More
Day 4: Looking Back, Looking Forward
Day 5: Learning to Remember
Day 6: The Mountaintop
Day 7: Slavery and Beyond
Day 8: Lessons to Bring Home
Day 9: Final Lessons

