Human Insulin-producing Cells Can Be Easily Induced to Replicate, Pitt Study Finds
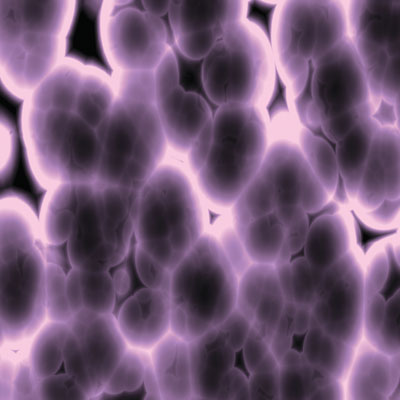
Researchers in the University of Pittsburgh School of Medicine have successfully induced human insulin-producing cells, known as beta cells, to replicate robustly in a living animal, as well as in the lab. The discovery not only could improve models and methods for studying diabetes, but it also opens up new possibilities for treating the condition.
“Most scientists thought that these important pancreatic cells could not be induced to regenerate, or could only replicate very slowly,” explained senior author Andrew F. Stewart, professor of medicine and chief of the Division of Endocrinology and Metabolism in the medical school. “This work provides proof-of-principle that the production of human beta cells can be stimulated, and that the newly generated cells function effectively both in the lab and in a living animal.”
The findings were published in Diabetes, one of the journals of the American Diabetes Association.
Lead authors Nathalie Fiaschi-Taesch, assistant professor in Pitt’s endocrinology division, and Todd A. Bigatel, a graduate of the postdoctoral fellowship program, identified molecules that play key roles in human beta, or islet, cell replication. They were building on previous work conducted by coauthor Irene Cozar-Castellano, also a Pitt instructor of endocrinology, who performed similar studies using mouse cells.
They found that, unlike rodents, human beta cells contain a significant amount of a protein called cdk-6. When cdk-6 production was increased using a viral vector carrying the cdk-6 gene, the cells replicated. Stimulation was further enhanced by increasing production of another cell cycle molecule called cyclin D1. Untreated human islets did not replicate.
“After we transplanted some of these engineered human beta cells under the outer layer of a kidney in a diabetic mouse, we saw that replication continued and blood sugar levels normalized,” explained Fiaschi-Taesch. “When we took out the kidney that contained the insulin-producing cells, the mouse immediately developed diabetes again.”
The prospect of being able to study human beta cells and their replication in vivo, meaning in a living animal, could greatly improve diabetes study models and could lead to techniques that generate new beta cells in patients with diabetes. In the future, it also could allow more effective therapeutic transplants of insulin-producing cells—either by expanding the numbers of cells available from a single cadaveric donor or from a gene-enhanced version of the patient’s own cells, or by establishing permanent cell lines from existing beta cells or stem cells, Stewart pointed out.
He added that cell cycle replication molecules might also be targets for drugs that could transiently turn on beta cell replication to increase insulin production.
The team’s work was funded by grants from the National Institutes of Health, the American Diabetes Association, and the Juvenile Diabetes Research Foundation.
Other Stories From This Issue
On the Freedom Road

Follow a group of Pitt students on the Returning to the Roots of Civil Rights bus tour, a nine-day, 2,300-mile journey crisscrossing five states.
Day 1: The Awakening
Day 2: Deep Impressions
Day 3: Music, Montgomery, and More
Day 4: Looking Back, Looking Forward
Day 5: Learning to Remember
Day 6: The Mountaintop
Day 7: Slavery and Beyond
Day 8: Lessons to Bring Home
Day 9: Final Lessons

