Pitt Researchers Present Findings During Tissue Engineering and Regenerative Medicine Meeting
Researchers in Pitt’s School of Medicine presented findings from more than a dozen studies during the Tissue Engineering and Regenerative Medicine International Society’s North American Chapter meeting, June 13-16 in Toronto.
Highlights of their findings follow.
Blood-forming stem cells cultured from human fat tissue
Pitt researchers have isolated and cultured human hematopoietic stem cells from fat, or adipose, tissue, suggesting that they have found another important source of cells for reconstituting the bone marrow of patients undergoing intensive radiation therapy for blood cancers.
Adipose tissue can rapidly expand or contract in accordance with nutritional constraints. In so doing, it requires rapid adjustment in its blood supply and supporting connective tissue, or stroma.
Based on previous reports that the “stromal vascular” fraction of adipose tissue contains stem cells that give rise to pericytes—cells surrounding small blood vessels—Pitt researchers, led by Albert D. Donnenberg, professor and director of the University of Pittsburgh Cancer Institute’s Hematopoietic Stem Cell Laboratory, isolated the stromal vascular fraction from human adipose tissue and expanded these cells by growing them in a specialized blood-culturing medium for 21 to 42 days.
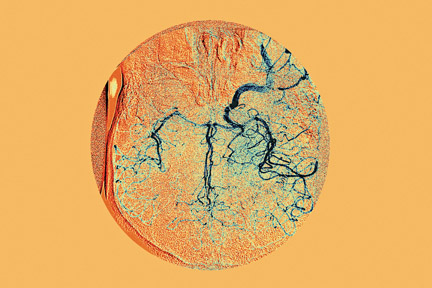
Using a cell-sorting method known as flow cytometry, the researchers detected a broad spectrum of blood-forming, or hematopoietic, cells among the cultured cells at varying stages of differentiation. In particular, they observed both early and mature red blood cells. Moreover, they detected CD34+ cells at approximately the same frequency as is present in freshly isolated bone marrow. In bone marrow, CD34+ expression indicates the presence of progenitor cells, which give rise to all of the different types of blood cells.
These data indicate that hematopoietic stem cells, or cells that give rise to them, are an integral part of normal adipose tissue, according to Donnenberg. “We took cells from the stromal vascular fraction of normal adipose tissue and basically gave them bone marrow food to see what would happen,” he said. “We were able to culture a variety of hematopoietic cells, including blood progenitor cells.”
Donnenberg said that using a patient’s own bone marrow or blood-derived stem cells for bone marrow reconstitution carries some risk that these cells are contaminated with the patient’s own tumor cells.
“Since it has been shown in some cases that tumor cells contaminating bone marrow grafts are the source of recurrent malignancies after autologous transplantation,” he explained, “this might be a way of giving patients who need bone marrow reconstitution their own hematopoietic cells derived from a source other than their defective bone marrow.”
“Off-the-shelf” vascular grafts developed by Pitt investigators
Investigators at Pitt have engineered artificial blood vessels from muscle-derived stem cells (MDSCs) and a biodegradable polymer that exhibit extensive remodeling and remain free of blockages when grafted into rats.
The results of their study have potentially significant implications for the treatment of heart and kidney diseases, in which there is a critical need for new sources of blood vessels for vascular grafts.
The saphenous vein taken from a patient’s leg continues to be the most commonly used graft for coronary artery bypass grafting even though a significant percentage of vein grafts eventually fail. Arterial grafts are the preferred conduits because they are less prone to becoming obstructed. However, they are in very limited supply, as many patients require multiple grafts. Thus, there is an ongoing search for the ideal small-caliber arterial substitute for revascularization procedures.
A Pitt team led by David A. Vorp, a professor of surgery and bioengineering and a faculty member of the McGowan Institute for Regenerative Medicine, developed its vascular graft by “bulk seeding,” or spraying, MDSCs inside a biodegradable porous, tubular polyester urethane scaffold using a rotational vacuum seeding device.
After culturing their vascular constructs for seven days, the investigators then implanted them in the abdominal aortas of rats eight weeks before performing tests to determine how well the grafts had performed. The cell-seeded constructs showed a significantly higher blockage-free rate than unseeded controls (55 percent versus 0 percent). In addition, at eight weeks, there was an extensive remodeling of the MDSC-seeded polymer by surrounding tissue, exhibiting tissue formation that is consistent with a mature artery.
According to Vorp, these findings in a rat demonstrate the feasibility of developing MDSC-seeded tissue-engineered vascular grafts for human application. “The next step is to demonstrate the use of the tissue-engineered blood vessel in a larger animal model, such as a pig, which has a coagulation system more similar to that in humans,” he said. “The advantage of our approach is that the graft could utilize the patient’s own stem cells and be ready for implantation almost immediately or, at most, after a relatively short culture period. This suggests that we could make these available ‘off-the-shelf,’ which is an essential element for clinical translation.”
Cancer stem cells similar to normal stem cells can thwart anticancer therapies
Current cancer therapies often succeed at initially eliminating most of the disease, including all rapidly proliferating cells, but are eventually thwarted because they cannot eliminate a small reservoir of multiple-drug-resistant tumor cells, called cancer stem cells, which ultimately become the source of disease recurrence and eventual metastasis.
Now, research by Pitt scientists suggests that for chemotherapy to be truly effective in treating lung cancers, for example, it must be able to target a small subset of cancer stem cells, which they have shown share the same protective mechanisms as normal lung stem cells.
The Pitt researchers, led by Vera Donnenberg, an assistant professor of surgery and pharmaceutical sciences, used cell surface markers and dyes to identify cancer stem cells as well as normal adult stem cells and their progeny in samples obtained from normal lung and lung cancer tissue samples. The scientists identified a very small, rare set of resting cancer stem cells in the lung cancer samples that looked and behaved much like normal adult lung tissue stem cells. Both the cancer and normal stem cells were protected equally by multiple drug resistance transporters, even if the bulk of the tumor responded to chemotherapy.
According to Donnenberg, the very fact that cancers can and do relapse after apparently successful therapy indicates the survival of a drug-resistant, tumor-initiating population of cells in many types of refractory cancers. “Because of the similarities between the way that normal stem cells and cancer stem cells protect themselves, cancer therapies have to be designed specifically to target cancer stem cells while sparing normal stem cells,” she explained.
Other Stories From This Issue
On the Freedom Road

Follow a group of Pitt students on the Returning to the Roots of Civil Rights bus tour, a nine-day, 2,300-mile journey crisscrossing five states.
Day 1: The Awakening
Day 2: Deep Impressions
Day 3: Music, Montgomery, and More
Day 4: Looking Back, Looking Forward
Day 5: Learning to Remember
Day 6: The Mountaintop
Day 7: Slavery and Beyond
Day 8: Lessons to Bring Home
Day 9: Final Lessons

